Some time ago, I attended a course titled, “Cone Beam Radiography: A Certification Program for Dentists” at UNLV taught by James Mah and Robert Danforth. It was very insightful and I thought I would share some of the main points with you.
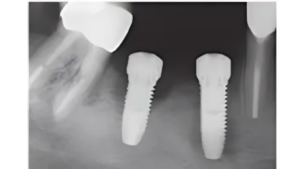
First, why should you care? By now, the benefits of CBCT are self-evident. We have all seen the tremendous benefits to virtually all areas of dentistry. You can visualize accessory canals for endo, localize impacted teeth, improve outcomes for implant surgery, and aid in orthodontic movement of teeth.
However, ordering CBCT images can sometimes be a little scary for us. Why? Because we know that we are liable for detecting irregularities that show up on the images. If we miss something in the images, we can be in serious trouble. As a result, I’ve heard of people ordering the smallest Field of View possible for every case. However, is this really to our patients benefit? Wouldn’t our health care delivery be improved if we trained ourselves to be competently and thoroughly screen these images? I think so.
Maybe some of us don’t want to “unnecessarily” expose our patient to radiation-so we might take a pano instead. I hope that the following information persuades you that these beliefs are unfounded and that we can significantly improve our patient care by not being afraid to take more CBCT images.
[mepr-show if=”loggedout”] Login or signup to Implant Ninja Dojo to read the rest of this article.[/mepr-show]
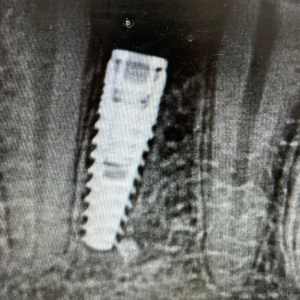
[mepr-show if=”loggedin”] Here is just one example (Courtesy of Dr. Mah) in which a CBCT would have saved the patient and clinician time, money, and pain. The patient presented for an implant placement #30, but it was first determined that a supernumerary tooth should be extracted from that site.

A general dentist attempted to extract the tooth, but was unable to even find it! Then an oral surgeon gave it a try but still was unable to even localize the supernumerary tooth. Finally, they decided to take a CBCT. This is what they saw:

It turned out to be a sialolith, not a supernumarary tooth at all! They would have known that if they had just taken a CBCT from the beginning.
CBCT is NOT Medical CT
A medical CT is very different from a Cone Beam (not groundbreaking information…I know). They both take tomographic images but the doses of radiation that the patient is exposed to are radically different for each.
So instead of telling your patient, “We are going to give you a CT scan” you might instead say, “We are going to take a comprehensive 3D image.”
Are the Doses Dangerous?
In North America, the average person is exposed to about 8micro Sieverts of radiation per day just from their environment. Of course, this value varies by geographic location–with urban areas often presenting much higher daily doses. You are exposed to radiation everywhere; you even get 10mSieverts from the potassium in a banana!
Let’s look at exposure from dental films for comparison. These values are expressed in microSieverts.
- Panoramic: 3-11
- Lateral Ceph: 5-7
- PA Ceph: 5-7
- Occlusal: 5
- Full Mouth Series: 30-80
- TMJ series: 20-30
- CBCT: 6-135
- MEDICAL CT: 10,000
The value for the Cone Beam varies widely because it can be operated under various settings that alter radiation exposure. For example, a standard scan of the Maxilla can expose the patient to 32mS, whereas a scan of both arches + the TMJ can expose the patient to 79 mS. (Ludlow and Walker Am J Orthod Dentofacial Orthop. 2013;144:802-17)
It is reasonable to say that the radiation exposure from CBCT is in the same range as dental films. Furthermore, a report from the National Council on Radiation and Protection Measurements (report #91) established that the risk of exposure from CBCT may be negligible.
A Few Technical Tips
The settings and Field of View of the CBCT image should match the clinical need. This means that you shouldn’t take the highest setting for every patient. Instead, here are some general voxel parameters for different clinical needs.
Voxel size setting recommendations for different procedures:
- Ortho and Orthognathic surgery ~.40mm
- Implants ~ .3mm
- Endo ~.10mm
- Endo fractures/accessory canals ~ 0.07mm
Additional tips:
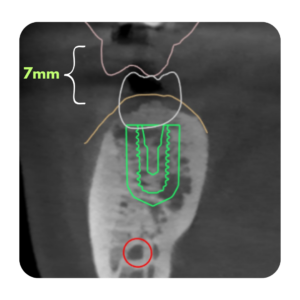
- Using a thyroid collar reduces exposure doses by about 50%
- In general, the smaller the Field of View, the higher the resolution.
- For a patient with a short/stiff neck, having them hold light weights during the scan can help you to lower their shoulders and thereby improve head position during the scan.
Irregularities in the Images
As CBCT is relatively new (introduced to the US in 2001) many of us have not received much training in CBCT interpretation in dental school. As such, we are responsible for training ourselves adequately to provide our patients adequate care in this arena.
There are many irregularities that may show up on these images. We do not necessarily have to be able to diagnose each and every one, but we should be able to notice when something doesn’t look right.
It is important to not only spot dental pathology, but we must screen all structures imaged, including all sinuses (maxillary, sphenoid and frontal), ethmoid air cells, airways, and the TMJ.
One common irregularity we will run into is calcifications. One study found that ⅓ or CBCT’s taken found them and that 90% were located in the upper neck. They can include tonsiloliths, sialoths, and calcifications of various ligaments or cartilage, and carotid artery calcifications.
You won’t learn to recognize these from reading an article, I think a great way to learn would be to buy a guidebook, such as The Atlas of Cone Beam Imaging for Dental Applications by Dale Miles and go over your own patient scans to learn the regular and irregular anatomy.
Thanks for reading! Cheers!
Ivan Chicchon [/mepr-show]

Responses