Hey there ninjas! Today, we’re diving into some seriously interesting dental lit. Let’s see if we can break it down complex topics into simple, actionable insights.
WARNING: Use these findings at your own risk. This research is legit. But it doesn’t mean you should go and immediately implement what you read. That’s not remotely close to how you should interpret research. Research is best when you spend time reading up consistently and utilize a wide body of literature and blend that with your own perspective from clinical experience to form opinions.
Understanding Anticoagulation Therapy
First things first, let’s talk about anticoagulation therapy. We’re talking about those widely prescribed medications that prevent and treat thromboembolism. Basically, they’re used to stop blood from clotting too much. These therapies are often prescribed to patients at risk of blood clots due to various medical conditions like heart diseases, strokes, and more.
The Heroes of the Game: Warfarin and Heparin
Now, in this anticoagulation universe, we’ve got some heroes – Warfarin and Heparin. These are like the MVPs of antithrombotic drugs.
Warfarin is taken orally, and it works on Vitamin K in the body to control clotting.
On the other hand, Heparin is often used in hospital settings and given through injections.
Surgical Adventures: Implants and Bleeding
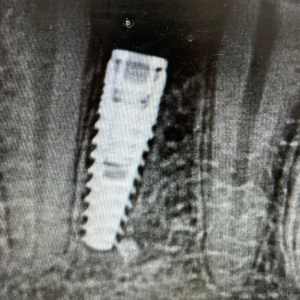
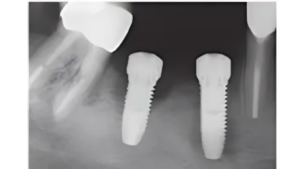
So, here’s where it gets interesting – dental implant surgery. Many patients are on anticoagulation therapy. So when you’re on anticoagulants, this can get a bit tricky. So, researchers have been exploring ways to handle this safely.
Local Hemostatic Agents: The Game-Changers
Enter the local hemostatic agents – these are super handy bleeding control tools. The study we’re talking about sought to understand which agent works best for implant surgery.
Think of it as choosing the perfect tool to keep the blood in check during surgery. They tried TXA (Tranexamic Acid), BS (Bismuth Subgallate), and DG (Dry Gauze) – all different ways to handle bleeding.
The Research Quest: What Went Down
Okay, here’s the scoop on the study. The researchers rounded up some patients needing dental implant therapy.
80 surgeries were split into 4 different groups based on the local hemostatic agent they’d use during surgery.
Group 1: control (not on any anticoagulants)
Group 2: TXA
Group 3: BS
Group 4: DG
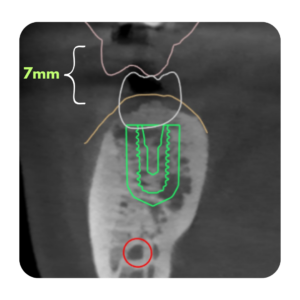
Before the surgery, the INR of patients on OAT was verified to ensure it was within the range of ≥ 2.0 to ≤ 3.5.
Implant surgery was performed. And it seemed like the authors followed fairly conservative surgical practices to carry out the procedures. For example, the didn’t use any vertical incisions in their flaps. It seemed like they tried to get in and out within minimal trauma.
Results
Drumroll, please!
Out of the 80 patients, 2 patients developed intraoral hematomas, 14 developed extraoral hematomas, and 2 patients had bleeding from the wound 1-5 days after the procedure that was easily controlled.
The study found that implant surgery for patients on anticoagulation therapy (with Warfarin) could be done safely without stopping their medication. They suggest you can perform dental implant surgery without putting the brakes on their therapy. Plus, they found that different hemostatic agents did a pretty good job at controlling bleeding. There was, however, an association between hematomas and alveolar ridge recontouring procedures.
Unveiling the Real Heroes: TXA and Friends
Now, here’s the deal – all the hemostatic agents worked well, but there were a couple of standouts. TXA, when soaked in gauze, turned out to be a superstar in controlling bleeding.
But it’s not the only option; others like DG and BS were also effective.
A Peek Into the Future: What’s Next?
Of course, this study isn’t the end of the road. There’s still so much to explore. Maybe we’ll see more research that involves a larger group of patients to confirm these findings. And as we move forward, we might discover even better ways to handle bleeding during surgeries, making implant procedures smoother and safer for everyone.
Final Thoughts:
The conclusion is that implant placement in patients on warfarin without stopping the anticoagulation treatment was safe in these particular cases, and the local agents used effectively managed bleeding. Hematomas were more likely with alveolar ridge recontouring.
HOWEVER, these are details upon which patients’ lives can depend. Just because this study claims this, it does not mean that it is safe to employ in your practice.
Not every clinician will be prepared to handle these cases. You will always want to carefully and conservatively vet your patients and only do procedures that you feel personally comfortable with given your training and clinical experience.
[metaslider id=”4939″]

Responses