Maybe you’ve been there. Your patient needs an extraction and you also tell them that they also need bone grafting in the socket because “it keeps your bone from shrinking.” The patient looks at the treatment plan price, and then asks you how much they really need the bone graft. This gets you to wonder if this ‘fairy dust’ that we sprinkle into extraction sites really makes that big of a difference.
I started to worry a little bit when I came across an article by Mardas et al. This systematic review found that there is NO clear evidence that socket grafting does any of the following:
1) increases implant placement feasibility
2) increases success of implants
3) maintains marginal proximal bone any better
They explain that the bone loss following an extraction was usually not severe enough to prevent the placement of an implant. In other words, the bone will NOT immediately vanish after the tooth is pulled so you will still be able to successfully place an implant.
[mepr-show if=”loggedout”] Login or signup to Implant Ninja Dojo to read the rest of this article.[/mepr-show]
[mepr-show if=”loggedin”]Well then, is there any benefit to socket grafting for implants? According to them, socket grafting at the time of extraction makes it less likely that additional grafting will have to be done at the time of implant placement.
Not exactly compelling evidence to use it in my practice, but let’s remember that these guys were looking only at how socket grafting affected implant success. Of course, implant success is necessary, but I am also concerned about the esthetic outcome of the case which can depend on the preservation of the alveolar ridge dimensions.
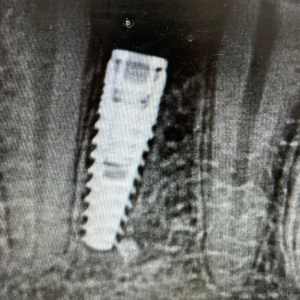
Then comes this wonderfully thorough article in the Journal of Prosthetic Dentistry, by Jambhekar et al. This systematic review shows that when it comes to maintaining ridge dimensions, socket grafting certainly does make a difference! In flap-less extractions, grafting helped to maintain bucco-lingual width and buccal wall height (after 12 weeks) much better than just allowing the socket to heal on it’s own.
Ungrafted sites had 2.7mm loss in B-L width and 1.74mm loss in ridge height. Compared to 1.3mm and 0.57mm, respectively with xenograft.
So once again, my confidence is restored in socket grafting.
But what type of graft should I use? The Mardas article claims that there is not enough evidence to say that any material is better than another. However, we can once again go to the Jambhekar article for further insight.
They show that allografts and xenografts were the best for maintaining ridge dimensions. However, these these graft materials also lingered in the sockets for a longer period of time and did not result in as much vital bone development when compared to alloplast material or no grafting at all. When it came to promoting the highest quality of bone (vital bone) alloplasts were the best.
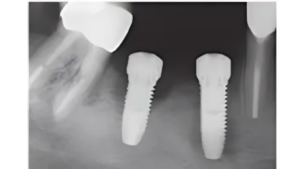
It is interesting to note that the bone preservation accomplished by xenografts was similar to the results obtained by Tarnow et al with extraction, immediate implant placement, and grafting. So, immediate placement should also be a valuable tool for you in preserving bone –but this is a whole other topic for a later article.
To sum it up:
For a posterior tooth, I am less likely to recommend socket grafting. This is because as long as an implant is to be placed in the near future (3-4 months), there should still be sufficient bone available.
Grafting in the esthetic zone is a HIGHLY complex matter and I will discuss some of the factors affecting decision-making in this area in subsequent post. I would, however, like to draw some useful generalities from these articles.
In the esthetic zone, I am more likely to recommend grafting with an extraction. Not because I am afraid I won’t be able to place an implant later–but because I want to preserve the ridge dimensions as much as possible. Also, if immediate implant placement is in your skillset, this is a viable option as well.
Now that we’ve (hopefully) justified our use of socket grafting, we will discuss evidence-based decision-making for anterior socket grafting in upcoming articles. This will attempt to describe the different scenarios you may face (missing buccal plate) and different patient biotypes and how you might manage their situations differently.
Thanks for reading! Cheers!
Ivan
References:
Nikos Mardas. Does ridge preservation following tooth extraction improve implant treatment outcomes: a systematic review. 2014
Jambhekar, et al. Clinical and histologic outcomes of socket grafting after flapless tooth extraction: A systematic review of randomized controlled clinical trials. 2015. JPD
Comment by Dr. Anders Nattestad (Oral Surgery):
Thanks Ivan,
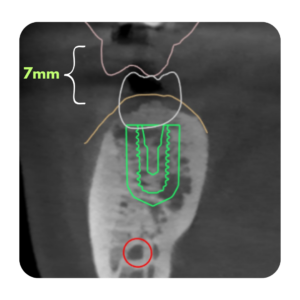
I appreciate your review and I agree with 60-70% of it. I agree with the posterior teeth not needing it and I do not like xenograft because they in my hands linger for too long. I like how the review is short and simple, but for me that is too simplistic for the anterior teeth, where there are a crucial pieces missing. Those are among others, the gingival biotype, any existing recession, smile-line, estethic demand of the patient and to me most important: the presence and state of the buccal plate. In some cases, an immediate implant is a good solution, but in other (depending on the analysis of the finer details) you may get some unpredictable soft tissue shrinkage around an immediately placed implant even if the buccal gap is grafted. In the last decade I am placing a few less anterior maxillary implants immediately, but more early after 8 weeks or so, and I am grafting allograft with membranes a little bit more (but then waiting 4-6 months before implant goes in). To help make decisions before you are in there, we like a small volume ICAT in those cases to evaluate the buccal plate ahead of time and the availability of palatal bone, should an immediate placement be a good option.
Complicated issue with lost of room for disagreement so just my 2c worth. One non-scientific issue here is that since some of these techniques are operator sensitive and you are doing something that works for you – that cannot be wrong as long as you document your cases well and does good follow-up, and are ready to change if your outcomes are not on par with the current trends.
Anders
BTW: Thanks for avoiding the term socket preservation, which is confusing and ridge preservation is a better term.[/mepr-show]

Responses