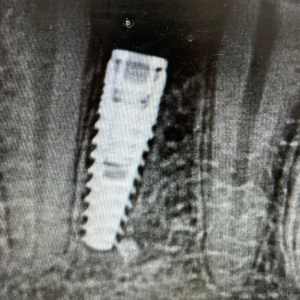
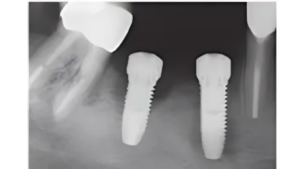
Per-implantitis remains an elusive foe. Progressively migrating bone loss around an implant, with some bleeding on probing and sometimes some pus, is an ailment that we are still battling with various methods.
Some people advocate mechanical debridement. Some advocate chemical cleansing. Some throw in both. Others swear by various cocktails, rabbits’ feet, and concoctions from unknown internet sources.
One controversial method of disinfecting an implant surface is known as implantoplasty. This entails mechanically removing the threads from the implant and turning that rough surface into a slick smooth titanium finish.
You basically take a high speed to the implant.
When I was in my prosthodontics residency, I brought this up to one of the faculty at the school. The response was, “What are those guys smoking?” It was sort of a crazy idea to cut on an implant.
Of course, there is more finesse to it the procedure than that. Everyone who does it has their own unique way. But so far we can agree that a diamond bur is used first and then an Arkansas stone is used to finish it off.
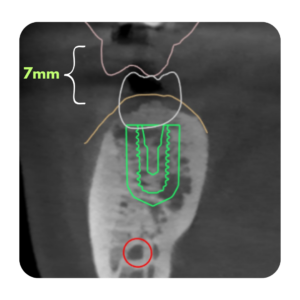
You have to be careful to use a lot of irrigation with saline, and be sure to not over-reduce the implant diameter because you don’t want to weaken it. For example, if you have a commercially pure titanium implant, and the implant is 3.2 mm in diameter, you might have a problem. Why? Commercially pure titanium is inherently weaker. And with such a small platform, you need all the thickness you can muster.
However, despite the controversy, the literature is showing that Implantoplasty does have a place in the battle against peri-implantitis.
Implantoplasty is proving to be more effective than other surgical interventions. MORE THAN 10% MORE EFFECTIVE!
Surgical approach without Implantoplasty: 81.7-86% long-term implant survival
Surgical approach with Implantoplasty: 94% for nonregeneration and 97% with regeneration
So, should you whip out your high speed every single time you see an exposed thread? Hold on there, probably not. Currently, it’s mostly reserved for defects that don’t have hope of regenerating or rebuilding bone. (Although some are also using implantoplasty in conjunction with building bone.)
But for now, we can at least say that it does seem to be effective in stopping bone loss and bleeding on probing in some advanced defects. Will this help the implant regain it’s bone? Maybe not. But at least it brings it back to health. And for molar implants, it can get patients back to chewing steak–and if that’s good enough for them it’s good enough for me.
Resources:
Chang HL, Lin GH, Suarez F, MacEachern M, Wang HL. Surgical management of peri-implantitis: A Systematic review and meta-analysis of treatment outcomes. J Periodontol 2014;85:1027-1041.
Ramel CF, Lussi A, Ozcan M, Jung RE, Hammerle CH, Thoma DS. Surface Roughness of dental implants and treatment time using six different implantoplasty procedures. Clin Oral Implants Res 2016; 27:776-781.
Heitz-Mayfield LJA Salvi GE, Momnelli A, et al. Supportive peri-implant therapy following anti infective surgical peri implantitis treatment: 5 year survival and success. Clin Oral Implants Res 2018;29:1-6.
Parma Benfenati S, Tinti C Romano F, Roncati M, Aimetti M. Long term outcome of surgical regenerative treatment of peri-implantitis: A 2-21 year retrospective evaluation. Int J Periodontics Restorative Dent 2020;40:487-496
Carcuac O, Derks J Abrahamsson I, Wennstroom JL, Petzold M, Berglundh T. Surgical treatment of peri-implantitis: 3-year results from a randomized controlled clinical trial. J Clin Periodontal 2017;44:1294-1303.
de Tapia B, Valles C, Ribeiro-Amaral T, et al. The adjunctive effect of a titanium brush in implant surface decontamination at peri-implantitis surgical regenerative interventions: A randomized controlled clinical trial. J Clin Periodontol 2019;46:586-596.
Cho-Ying Lin, Zhaozhao Chen, Hong-Lin Chiang, Whei-Lin Pan, Hom-Lay Wang, The Impact of Implantoplasty in Regenerated and Nonregenerated Treatment Modalities in Peri-implantitis: A Systematic Review and Meta Analysis , International Journal of Oral and Maxillofacial Implants, Vol 37,2021.


Responses
Can you elaborate on the technique for this? Have you tried this, and what results have you had?
Hi Grace! Thanks for asking. I’ve done this a handful of times.
1.Reflect a flap
2. De granulated the implant surface. This is the most tedious part as granulation tissue likes to stick to the surface. You can look into something called a “I brush” or “r brush” to help you remove it.
3. Remove the implant threads.
I have used a football bur on an electrical handpiece while my assistant blasts sterile saline on the implant.
4. Smooth the surface. I have used brownie greenie points (the kind that used to be used to polish amalgam.) but people now are using a white bur called an Arkansas stone.
@implantdr
The results I have seen is: it does help with inflammation. So basically the implants still have bone loss—but at least the tissue doesn’t look terrible any longer. The tissue starts to look healthier.
If you combine this with a renewed oral hygiene at the implant site, it can make the situation much better.