This is Part I, Case 2 in a series of cases that I completed, documented, and submitted for dental implant credentialing exams. I strongly believe in the value of credentialing exams to learn from a group of likeminded dentists, showcase your own knowledge to your staff, patients, and colleagues, and help promote quality dental implant care in the dental community.
I hope that sharing these case reviews will help others prepare for the AAID/ABOI Oral Exams and Case Presentations as well as showcase a good variety of implant cases to learn from. The posts will mimic the exact template of submitted cases for their respective exams. The breakdown of cases for this series will be spread out over the next several months but here is an outline of cases to look forward to reviewing:
- Part 1: AAID (American Academy of Implant Dentistry) Associate Fellow Exam
- Case 1: Single Tooth Implant
- Case 2: Quadrant Implant Case
- Case 3: Full Arch Implant Case
- Part 2: ABOI (American Board of Oral Implantology) Diplomate Credentialing Exam
- Case 1: Implant Overdenture
- Case 2: Lateral Sinus Lift and 2 Implants
- Case 3: Single Implant in the Esthetic Zone
- Case 4: Immediate Implant
- Case 5: Fixed Full Arch All-on-X
- Case 5: Edentulous Quadrant with 2 or more implants
- Case 7: Horizontal Ridge Augmentation and 2 Implants
- Case 8: Candidate Choice (Guided Overdenture)
The Case
History
Patient is a 68 year old caucasian male who presents for a regular recall hygiene visit with a chief concern of “I had a toothache on my lower left three weeks ago but it has gotten better.” The lower left second molar is missing and the lower left first molar has a porcelain crown and is root canal treated. Pain is mostly after eating per patient
Clinical and Radiographic Evaluation



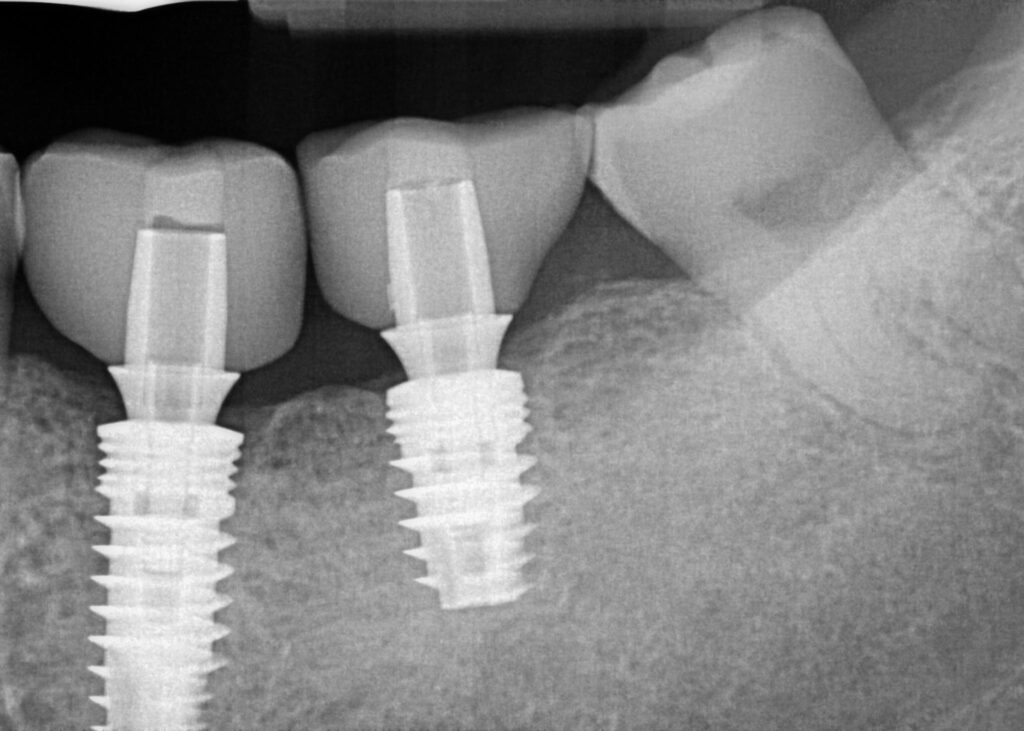
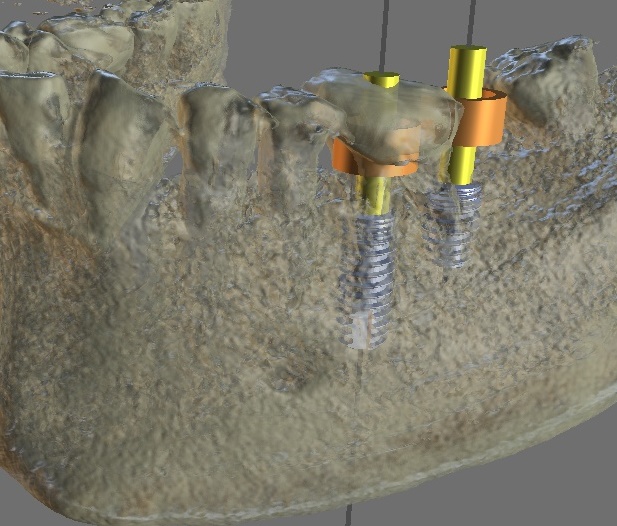
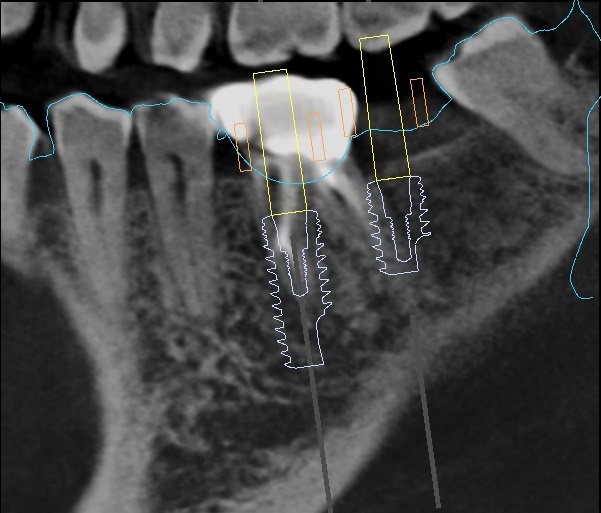
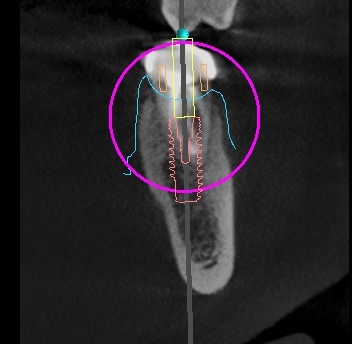
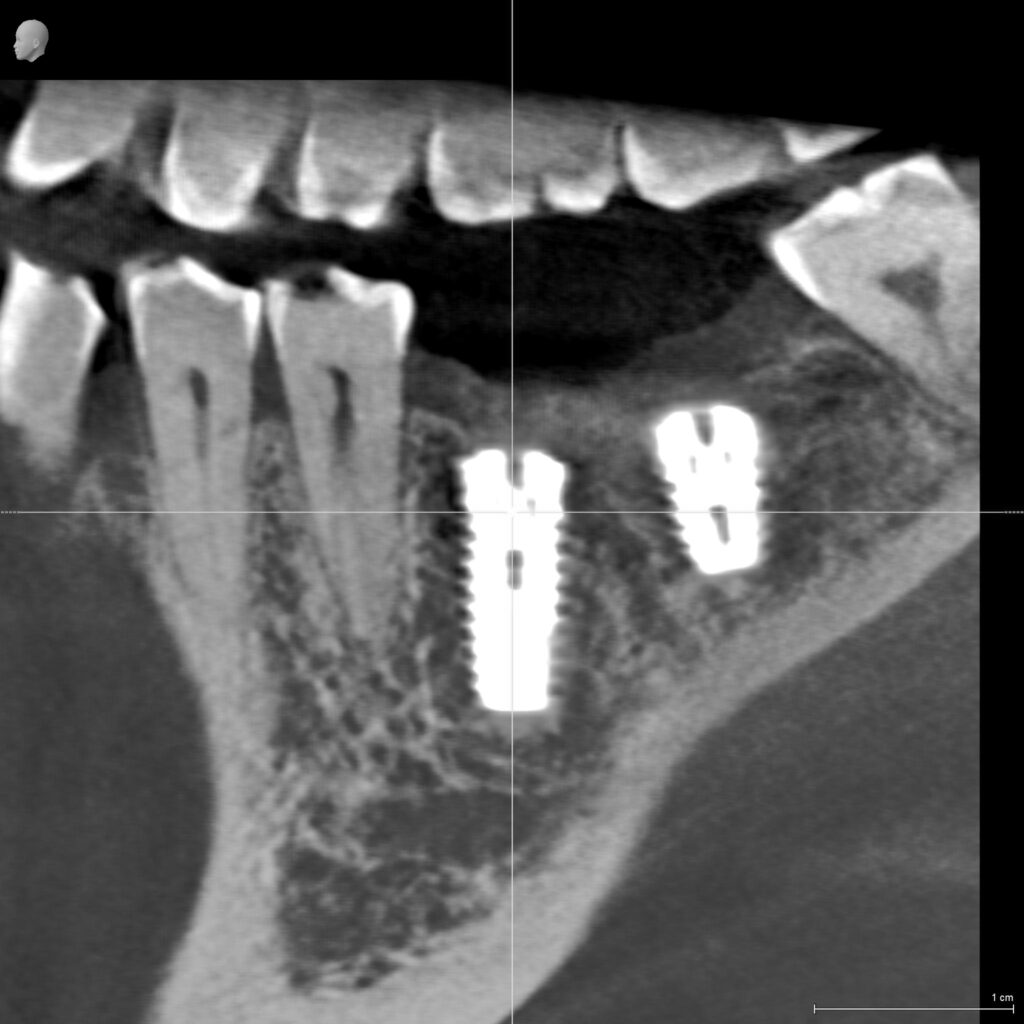
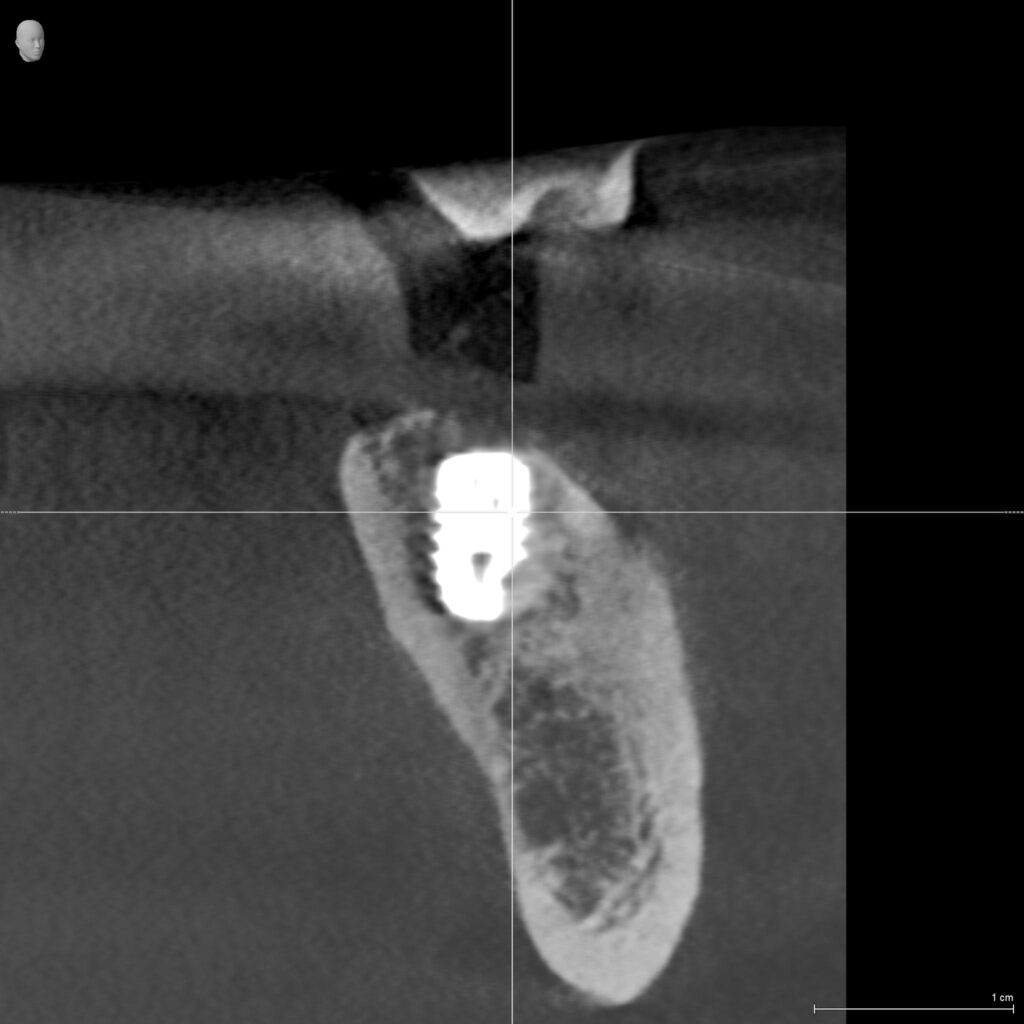
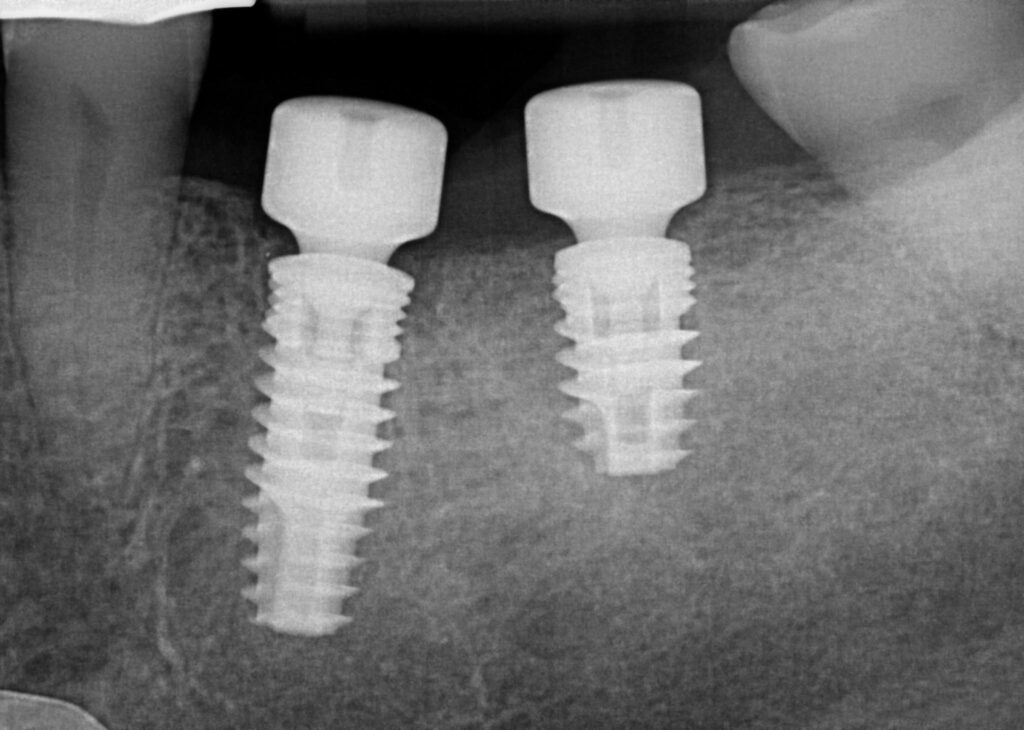
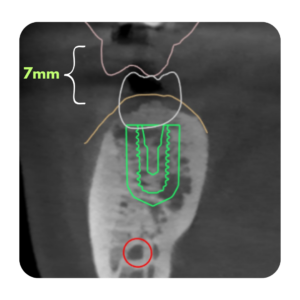
Periapical radiograph was exposed in the area of the lower left first molar. Radiographic exam revealed deep root caries at the margin of the build up material on the distal-buccal of the lower left first molar. No periapical infection or radiolucency is present. Previous conebeam computed tomography shows presence of the inferior alveolar neurovascular bundle to be 16mm from furcal bone of the lower left first molar and intact buccal and lingual plates. Adequate width and height in the lower left second molar site as well.
Diagnosis: Patient was diagnosed with partial edentulism (Kennedy class III) in the lower arch and recurrent caries on the lower left first molar. Tooth was diagnosed as non-restorable without surgical crown lengthening and new prosthetic. No infections are present.
Treatment Planning
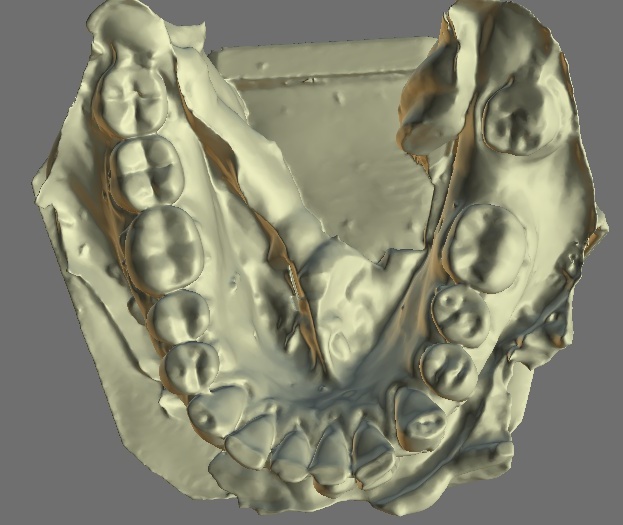
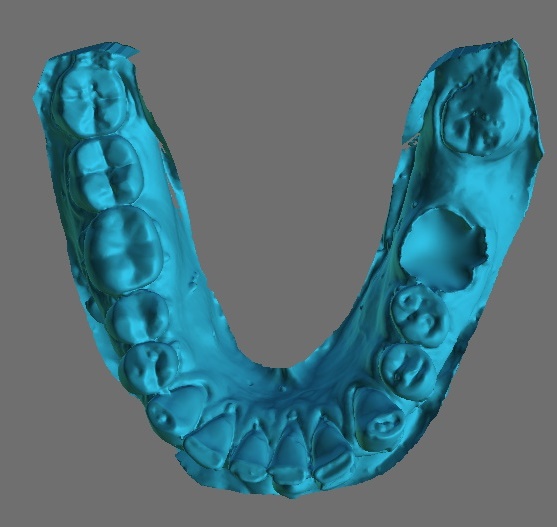

Patient’s chief concern was comfortable chewing. Once revealed that the lower left first molar was non-restorable the patient was interested in options to restore the lower left quadrant. Due to the long span between the third molar and the second premolar it was recommended that a fixed bridge not be chosen. A removable partial denture with a unilateral edentulous site was considered but patient wanted a non-removable option. An immediate dental implant with the extraction of the lower left first molar and a simultaneous placement of a dental implant in the healed site of the lower left second molar was the final treatment plan, which the patient accepted.
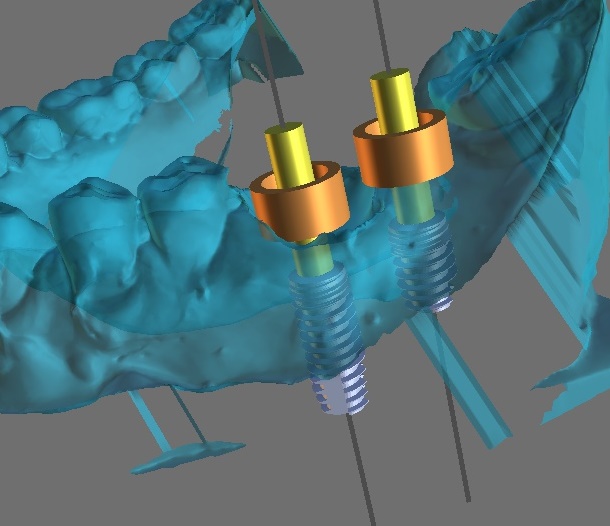
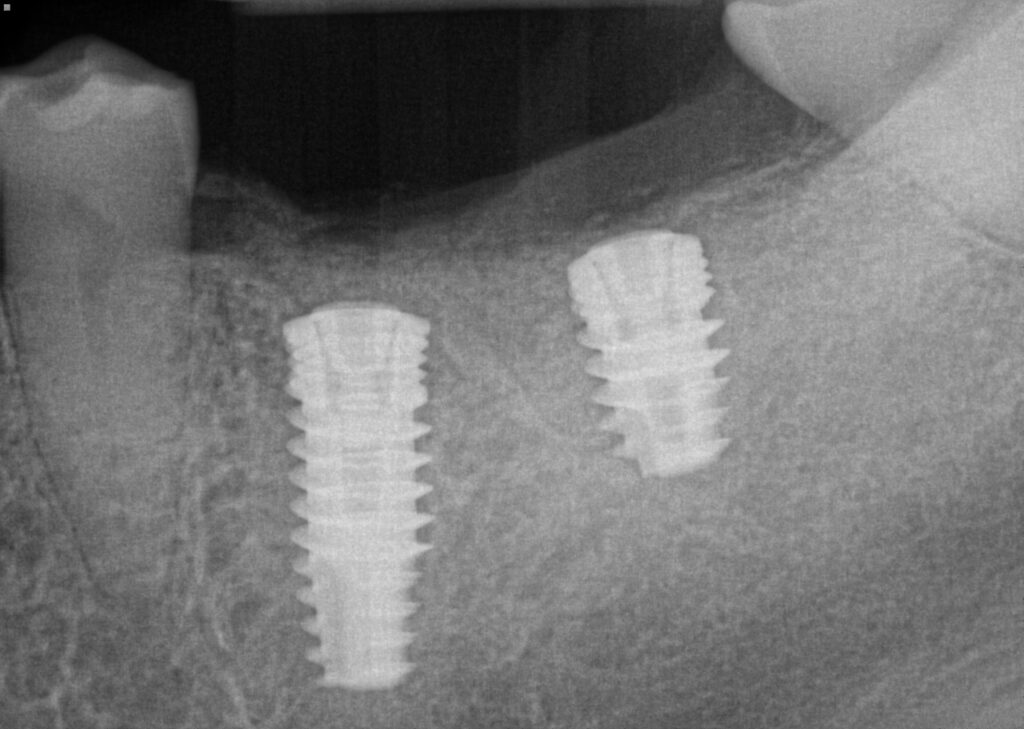
The the immediate implant in the lower left first molar a 5x13mm implant was chosen. The width was chosen due to ample width of the residual ridge and the history and signs of parafunctional habits. The length was chosen to engage 4mm apical to the extraction socket as well as the mesial and distal cribiform plate of the mesial root socket. The lower left second molar site was restored with a 5x8mm dental implant for the same reasons as the lower left first molar except the bone height above the inferior alveolar nerve bundle was 11mm and adequate healed hard tissue ridge was available for secure fixture of the 8mm long implant.
Surgical Appointment
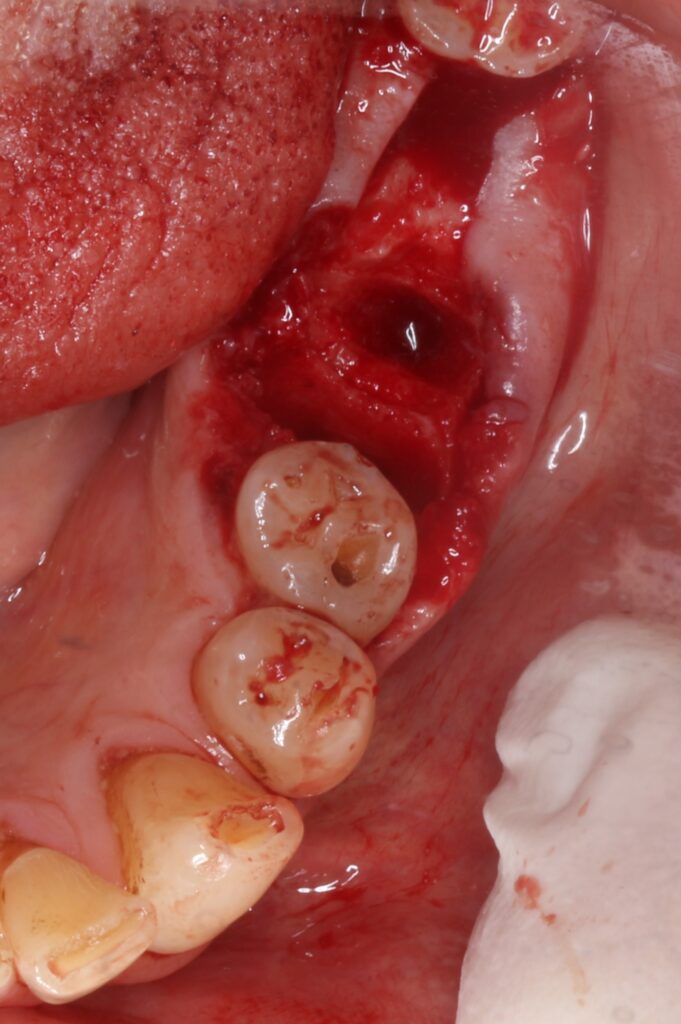

Patient presents for extraction of lower left first molar and placement of dental implants in the lower left first and second molar sites. 2 carpules of 4% septocaine 1:100k epinephrine, 1 carp in IAN block and 1 carp infiltration buccal and lingual to sites. Tooth was elevated, luxated, sectioned, and removed in two pieces. No damage noted to the buccal or lingual plates.
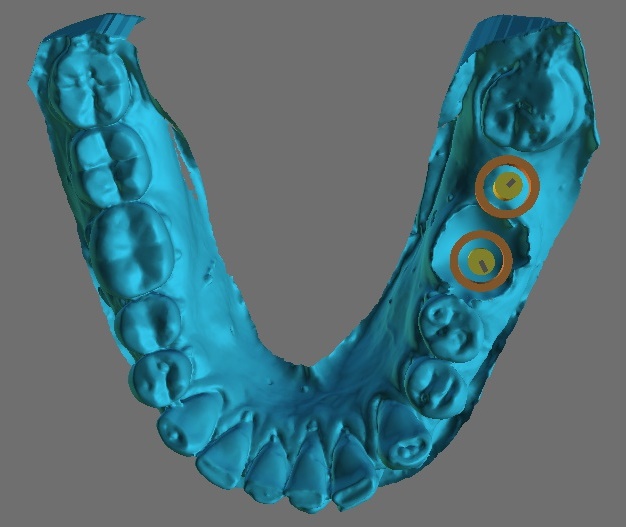
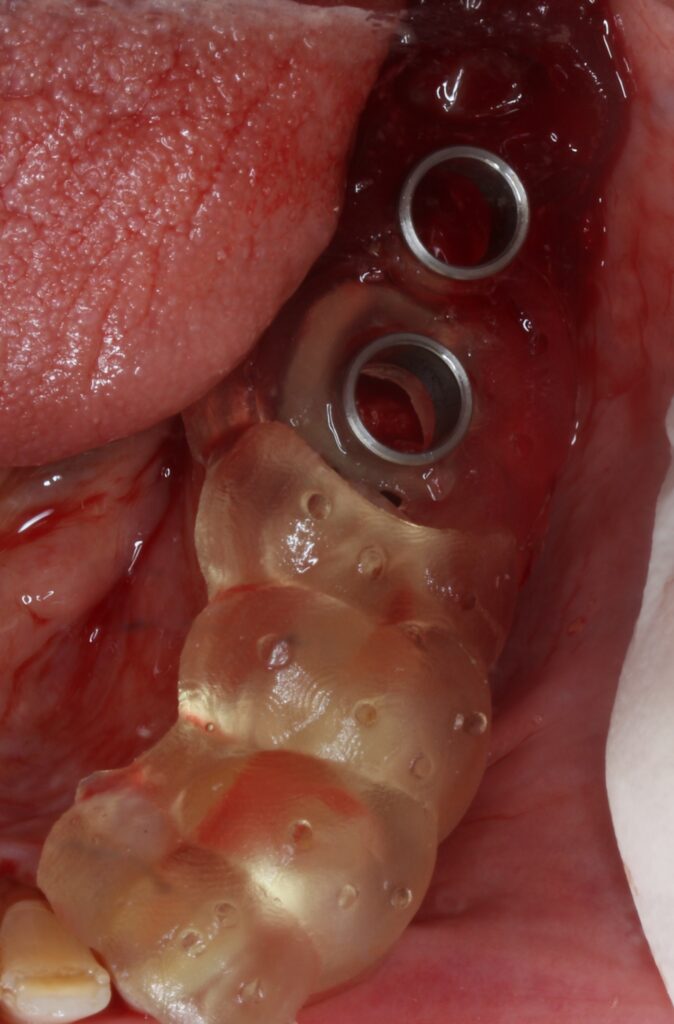
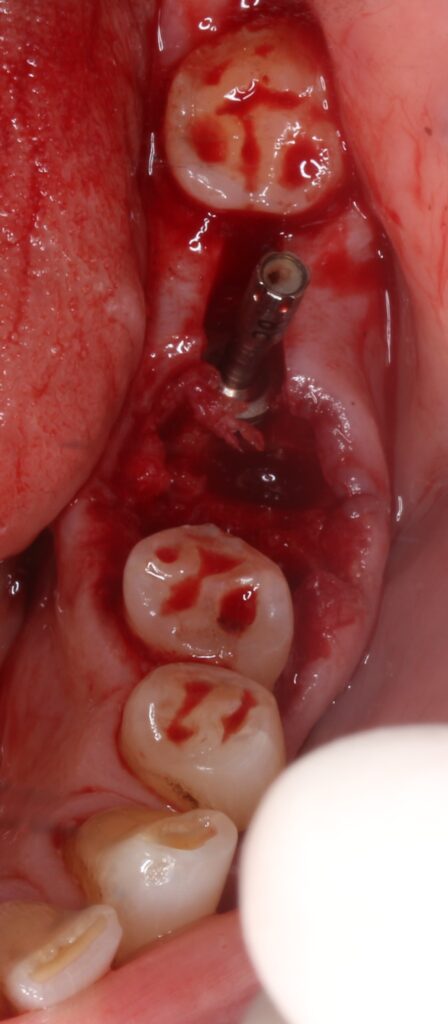
Guide seat confirmed visually. Guided 2.0, 2.5, 3.2, 3.7, and 4.3mm osteotomy drills utilzied through the guide with copious irrigation for the mesial root socket site of the lower left first molar and the healed ridge in the lower left second molar site. Chlorhexidine flush in each osteotomy prior to implant placement. 5x13mm Blue Sky Bio Bio|Max dental implant placed through the guide in the mesial socket of the lower left first molar. Timing and final depth confirmed with guide removed. 5x8mm Blue Sky Bio Bio|Max dental implant placed in the healed site of the lower left second molar. Timing and final depth confirmed with guide removed. ISQ 77 lower left second molar and ISQ 78 lower left first molar, both torque >30Ncm
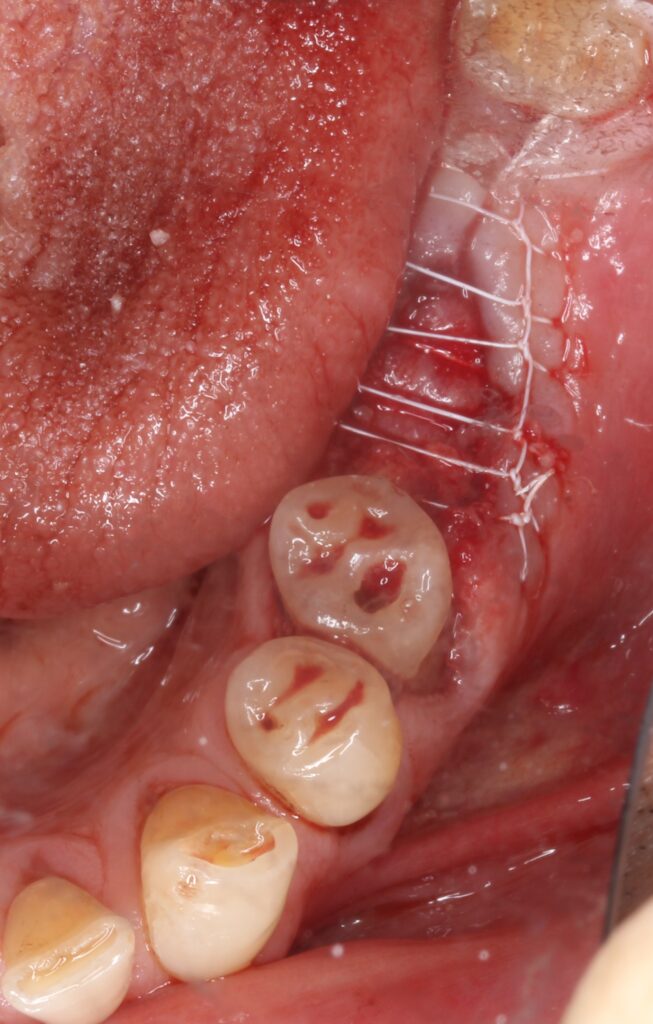
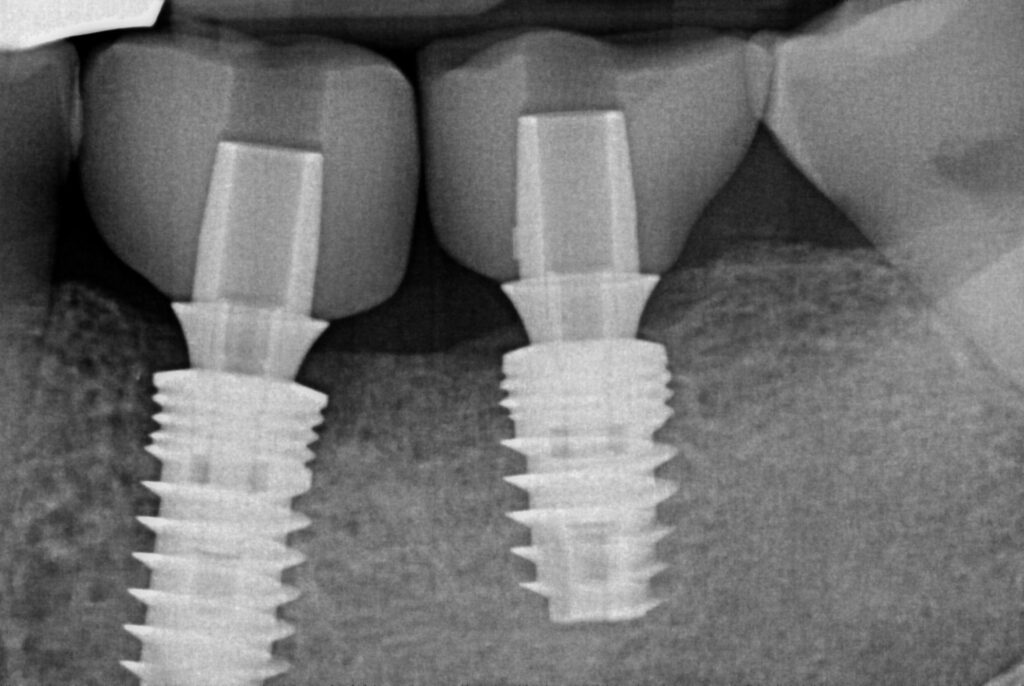
Chlorhexidine rinse of implant connection and cover screws placed. Bone graft 50:50 corticocancellous allograft placed in previous socket space and around. 20x30mm pericardium membrane placed over both sites and tucked into buccal and lingual flaps. Slight flap release around the lower left first molar site, continuous double-interlocking PTFE sutures. Post op PA and Quadrant CBCT taken and ideal placement confirmed prior to patient release.
NV: 2 week followup and suture removal.
Prosthetic Procedures



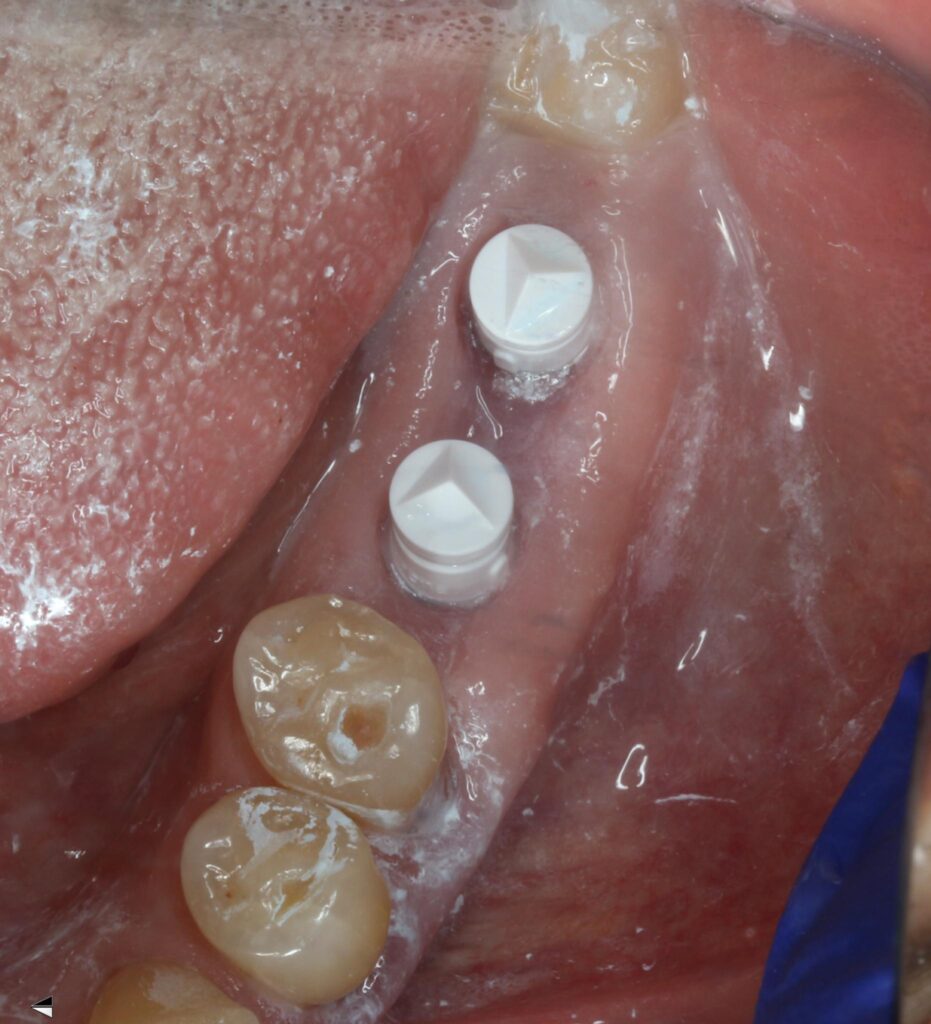

Patient presents for uncovery of implants in lower left quadrant. 2 carp 4% septo 1:100k epi infiltration. Full thickness flap mid crestal splitting the keratinized tissue, exposed both implant cover screws. Cover screws removed, chlorhexidine flush of implant body, healing abutments placed today, no sutures.
ISQ 84 and 81 for lower left second and first molar, respectively.
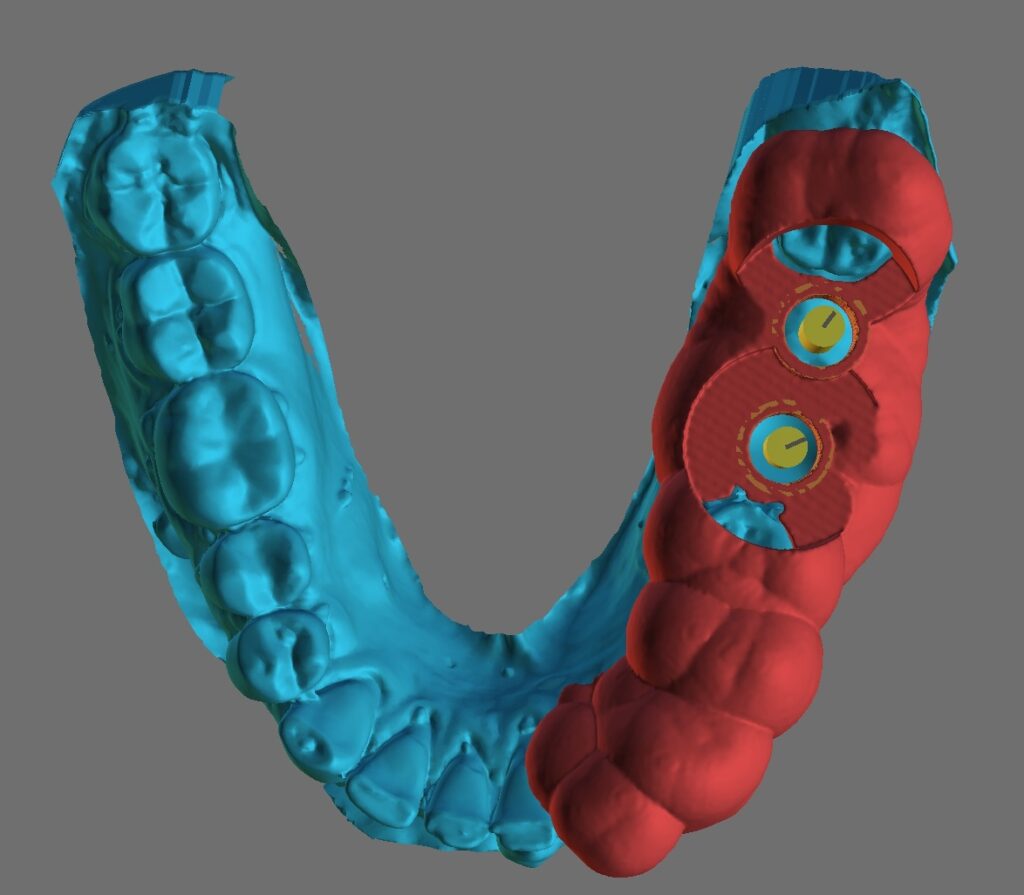
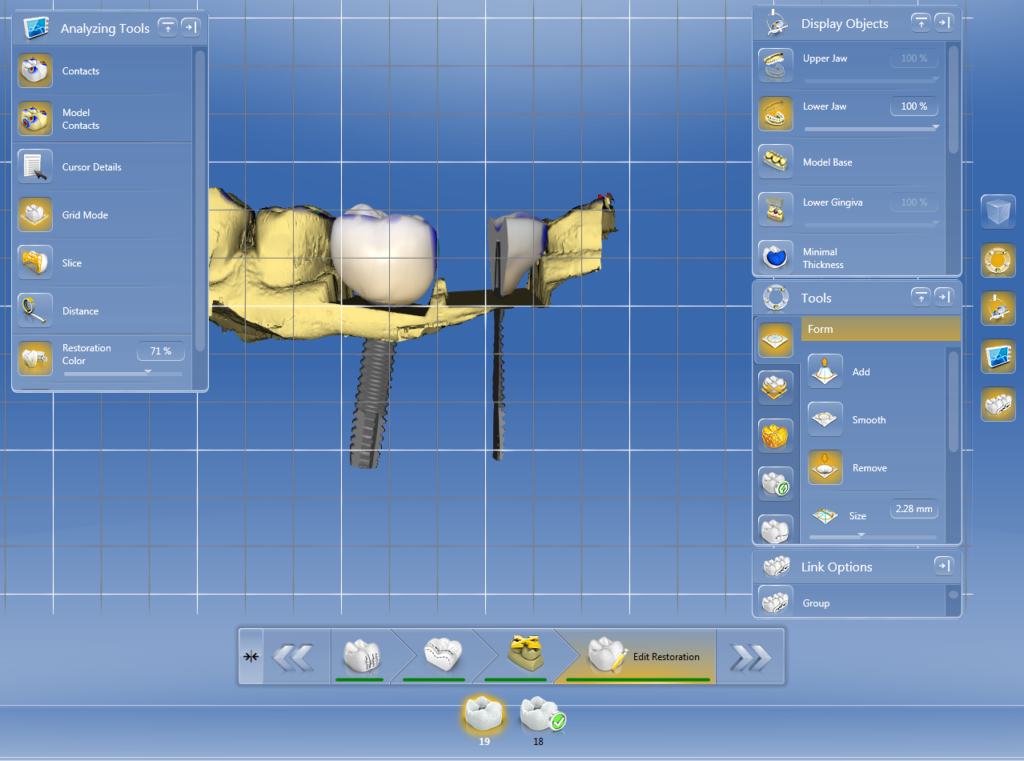
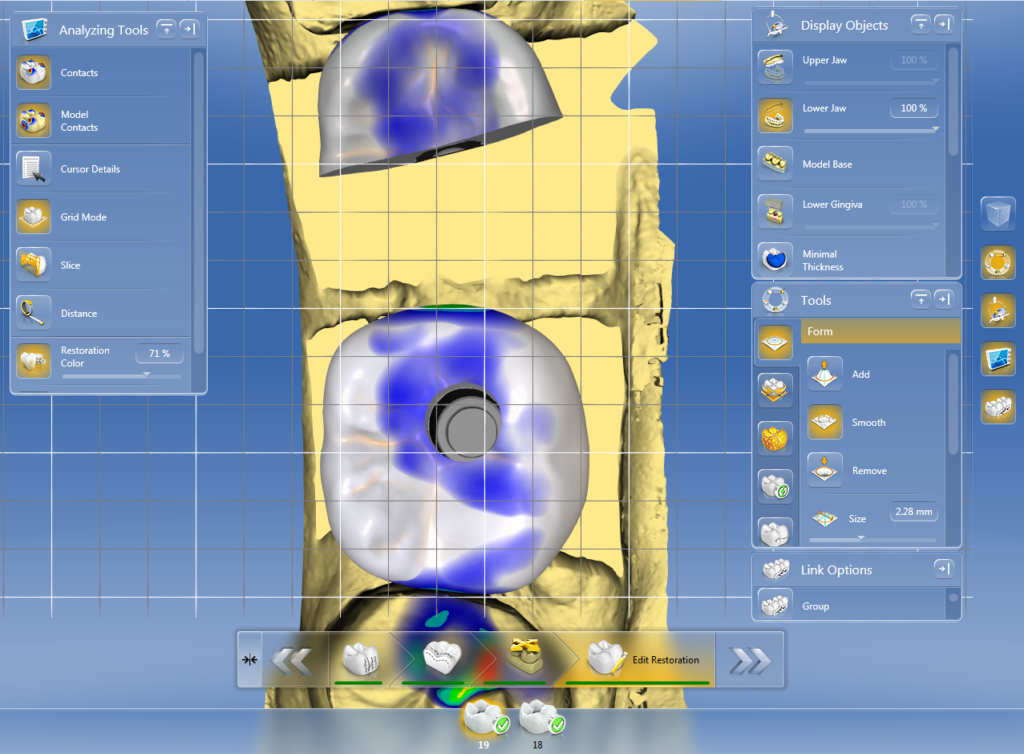
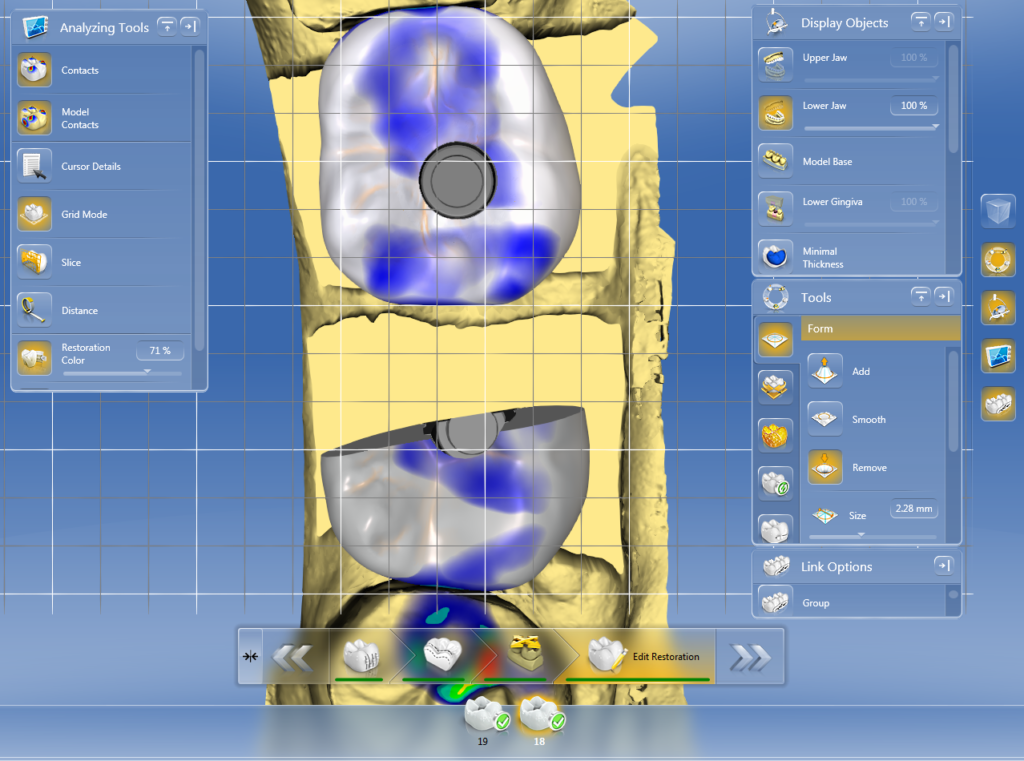
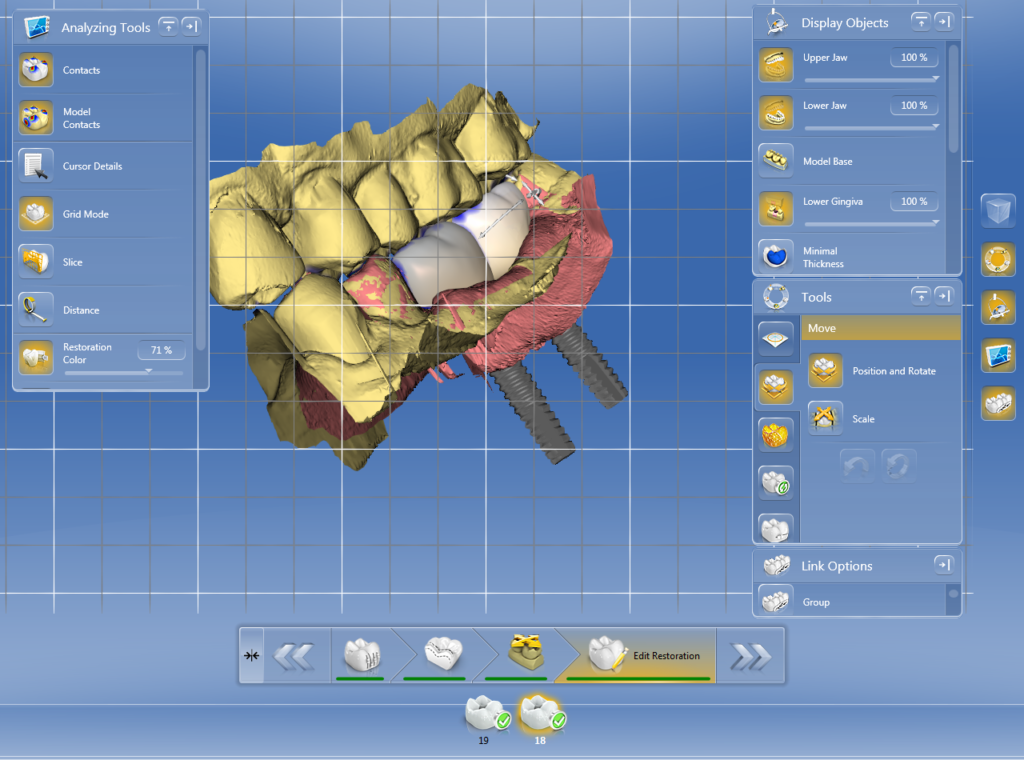
3 weeks later patient in for final impression with Sirona Cerec. Prep arch scan, opposing, bite, and final impression scan with sirona tibase and scan body. Final shade A3, Emax crown on hybrid abutment (screw retained).
Crowns luted outside of the mouth, cement margin cleaned and polished. Implant crowns placed and torqued to 30Ncm. Confirmed full seat with PA radiographs, confirmed contact and occlusion, removed excursive interferences.




Responses
Do you still irrigate your osteotomy and 2nd stage surgeries with CHX?
Yes that or saline, honestly whichever is loaded in the monoject syringe I don’t care either way. I do not have my patients use it themselves post operatively for at least 3 days so it doesn’t interfere with gum healing (even though in my experience it’s minimal), but irrigation before placement I still do without concern